Introduction
Cancer is one of the most pressing health challenges globally, affecting millions and their families each year. The pursuit of effective treatments has led to the development of remarkable best anti-cancer medicines tailored to combat various forms of cancer. This guide provides an in-depth look at the latest advancements in anti-cancer therapies, their mechanisms of action, and their impact on patient outcomes. As cancer treatment continues to evolve, understanding these options is essential for patients, caregivers, and healthcare professionals. Whether you’re seeking information for personal use or to support a loved one, this guide will equip you with valuable insights into the best anti-cancer medicines available today.
What is Cancer? Understanding Its Treatment
Cancer is characterized by the uncontrolled growth of abnormal cells that can invade surrounding tissues and spread throughout the body. Treatment options for cancer typically include surgery, radiation, and medications. Among these, best anti-cancer medicines play a crucial role in management. These medicines are generally categorized into chemotherapy, targeted therapy, immunotherapy, and hormone therapy. Chemotherapy employs powerful drugs to eliminate rapidly dividing cancer cells, while targeted therapies focus on specific molecular targets associated with cancer. Immunotherapy harnesses the body’s immune system to combat cancer, and hormone therapy blocks hormones that promote the growth of certain cancers. Gaining insight into these treatment modalities is vital for making informed decisions regarding cancer care.
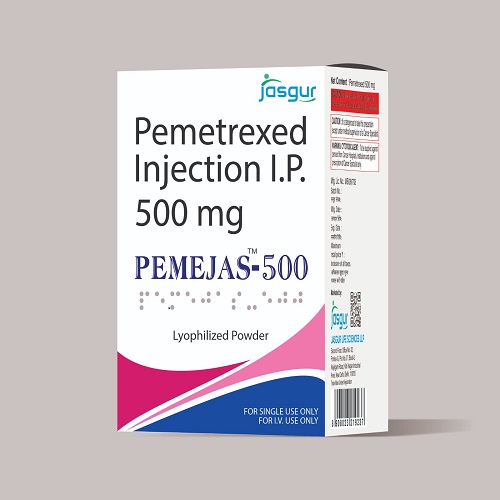
Chemotherapy: A Time-Tested Treatment
Chemotherapy remains a fundamental approach to cancer treatment and is often regarded as one of the best anti-cancer medicines available. It involves administering cytotoxic drugs that target rapidly dividing cells, a hallmark of cancerous growth. Chemotherapy can be delivered orally or intravenously and is typically given in cycles to allow the body to recover. While chemotherapy is effective in shrinking tumors and preventing the spread of cancer, it can also harm healthy cells, leading to side effects like nausea, fatigue, and hair loss. Despite these challenges, many patients find that the benefits of chemotherapy justify its use. Continuous research aims to enhance chemotherapy regimens, making them more effective and less toxic. By integrating chemotherapy with other treatment modalities, healthcare providers can improve patient outcomes and provide comprehensive care.
Targeted Therapy: Precision in Treatment
Targeted therapy has revolutionized cancer treatment, establishing itself as one of the best anti-cancer medicines available. Unlike traditional chemotherapy, which affects all rapidly dividing cells, targeted therapies zero in on specific molecular characteristics of cancer cells. For instance, drugs such as trastuzumab specifically target the HER2 protein in breast cancer, while imatinib inhibits the BCR-ABL fusion protein in chronic myeloid leukemia. This precision reduces side effects and enhances efficacy. As we deepen our understanding of cancer genetics, the development of novel targeted therapies continues to expand. Molecular profiling of tumors allows healthcare providers to customize treatments for individual patients, maximizing the likelihood of successful outcomes. Targeted therapies are increasingly becoming a standard part of treatment plans, further improving the precision and effectiveness of cancer care.
Immunotherapy: Empowering the Immune System
Immunotherapy has emerged as one of the most promising advancements in cancer treatment, solidifying its place among the best anti-cancer medicines. This innovative approach boosts the body’s immune response to recognize and destroy cancer cells. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, work by blocking proteins that prevent immune cells from attacking tumors. Additionally, CAR T-cell therapy involves modifying a patient’s T cells to better target and eliminate cancer cells. Immunotherapy has proven highly effective in treating various cancers, including melanoma, lung cancer, and certain hematological malignancies. While not every patient responds to immunotherapy, ongoing research aims to identify biomarkers that can predict treatment effectiveness and improve patient selection. The potential for immunotherapy to yield durable responses and long-lasting remissions represents a new frontier in cancer care, offering renewed hope to many patients.
Hormone Therapy: Targeting Hormone-Dependent Cancers
Hormone therapy is a critical component of treatment for hormone-sensitive cancers, particularly breast and prostate cancers. Recognized as one of the best anti-cancer medicines, hormone therapy works by blocking or lowering hormone levels in the body, which deprives cancer cells of the hormones they need to grow. For example, medications like tamoxifen and aromatase inhibitors are commonly used in breast cancer treatment to block estrogen’s effects. In prostate cancer, androgen deprivation therapy (ADT) reduces testosterone levels, limiting cancer progression. Hormone therapy can be applied in various contexts, including as adjuvant therapy after surgery or as part of palliative care. While hormone therapy may not be suitable for all cancer types, it can significantly enhance outcomes for patients with hormone-sensitive cancers. Ongoing research continues to explore combination therapies that integrate hormone therapy with other modalities to improve effectiveness and reduce resistance.
Combination Therapy: A Holistic Approach
Combination therapy involves utilizing multiple treatment modalities to maximize effectiveness, positioning it as one of the most effective strategies among the best anti-cancer medicines. By integrating chemotherapy, targeted therapy, immunotherapy, and hormone therapy, healthcare providers can leverage different mechanisms of action to combat cancer cells from various fronts. This approach has shown remarkable success in managing complex and aggressive cancers, where single-agent therapies may fall short. For instance, combining immunotherapy with chemotherapy has yielded promising results in certain lung and bladder cancers, leading to higher response rates and improved survival outcomes. Ongoing clinical trials are exploring various combinations to optimize treatment strategies and broaden eligibility for patients. The future of cancer care lies in personalized combination therapies tailored to individual patients, enhancing efficacy while minimizing side effects.
Managing Side Effects of Anti-Cancer Medicines
While the best anti-cancer medicines can save lives, they often come with side effects that can affect a patient’s quality of life. Chemotherapy is notorious for causing nausea, fatigue, hair loss, and an increased risk of infection due to its impact on healthy cells. Targeted therapies may lead to specific side effects related to the targeted pathways, such as skin rashes or gastrointestinal issues. Immunotherapy can trigger immune-related adverse events, including inflammation of healthy organs. Effectively managing these side effects is essential for maintaining patient comfort and adherence to treatment. Healthcare providers play a crucial role in monitoring and addressing side effects through supportive care measures, including anti-nausea medications, growth factors, and lifestyle adjustments. Educating patients about potential side effects and encouraging open communication with healthcare teams can empower patients to manage their treatment journey more effectively.
The Role of Clinical Trials in Advancing Cancer Treatment
Clinical trials are vital for the development and approval of new best anti-cancer medicines. These trials assess the safety and efficacy of innovative therapies, providing essential data that shape treatment guidelines. Patients who participate in clinical trials may gain access to groundbreaking treatments not yet available to the general public. Additionally, clinical trials contribute to a deeper understanding of cancer biology, helping researchers identify new therapeutic targets and strategies. The journey from laboratory to clinical application for new anti-cancer medicines is rigorous, involving multiple testing phases to ensure patient safety and treatment effectiveness. Patients considering clinical trial participation should discuss their options with healthcare providers, who can offer guidance and support. A commitment to research and clinical trials is crucial for advancing cancer care and improving patient outcomes.
Support Resources for Cancer Patients
Navigating a cancer diagnosis and treatment can be overwhelming, making access to support resources vital for patients and their families. Numerous organizations and support groups provide valuable information about the best anti-cancer medicines, treatment options, and coping strategies. Resources such as the American Cancer Society and Cancer Support Community offer educational materials, counseling services, and peer support networks. Healthcare providers also play a critical role in connecting patients with resources that address their unique needs. Supportive care, including nutritional counseling, pain management, and mental health services, can enhance the overall treatment experience. Empowering patients with knowledge and support fosters resilience during their cancer journey. Open communication with healthcare teams and seeking available resources can significantly improve patients’ experiences and outcomes.
The Future of Anti-Cancer Medicines: What Lies Ahead
The future of cancer treatment is bright, with ongoing research and innovations leading to the next generation of best anti-cancer medicines. Advances in genomics and personalized medicine are enabling more tailored approaches to cancer care, allowing for the development of therapies that target specific genetic mutations. Additionally, the integration of artificial intelligence and machine learning in drug discovery is accelerating the identification of new therapeutic candidates. Combination therapies that utilize various treatment modalities are being explored to enhance efficacy and overcome resistance. Furthermore, the potential for preventive strategies, including vaccines and lifestyle interventions, is gaining traction in the fight against cancer. As we move forward, a multidisciplinary approach that combines research, clinical practice, and patient engagement will be essential for advancing oncology and improving patient outcomes.
Conclusion
The landscape of cancer treatment is continuously evolving, with the best anti-cancer medicines leading the charge in this progress. From chemotherapy and targeted therapies to immunotherapy and hormone therapy, each approach plays a crucial role in the battle against cancer. Understanding these treatment options empowers patients and their families to make informed decisions about their care. Ongoing research, clinical trials, and patient support are essential for advancing cancer treatment and improving outcomes. As we continue to explore new innovations and strategies, hope remains a powerful ally in the journey toward conquering cancer.